· By Keryce Henry
Crohn's Disease 101: What You Need to Know
Crohn’s disease is an inflammatory disease that affects the GI tract. It can affect almost anyone—while symptoms usually appear in men and women roughly equally between the ages of 20 to 35, there have been cases in children and adolescents too. An estimated three million Americans have been diagnosed with Crohn's.
We’ll be honest: Crohn’s disease can be scary and overwhelming when you’re not clear on exactly what it is. We’re here to help you understand a little more about this condition, its symptoms, and possible ways to treat it.
Remember: If you are experiencing uncomfortable bowel movements or blood in your stool, tell your doctor! You’ll be glad you did.
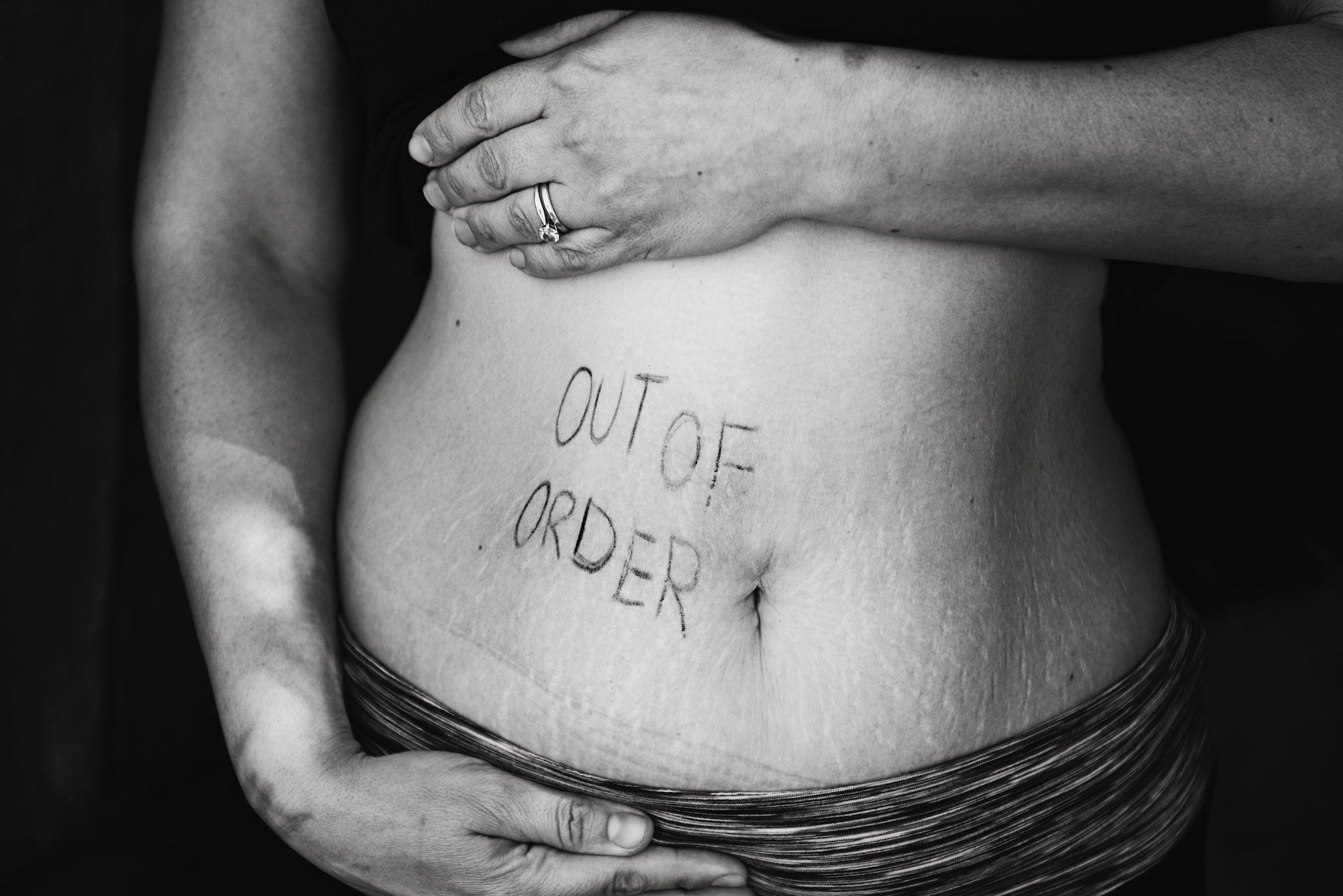
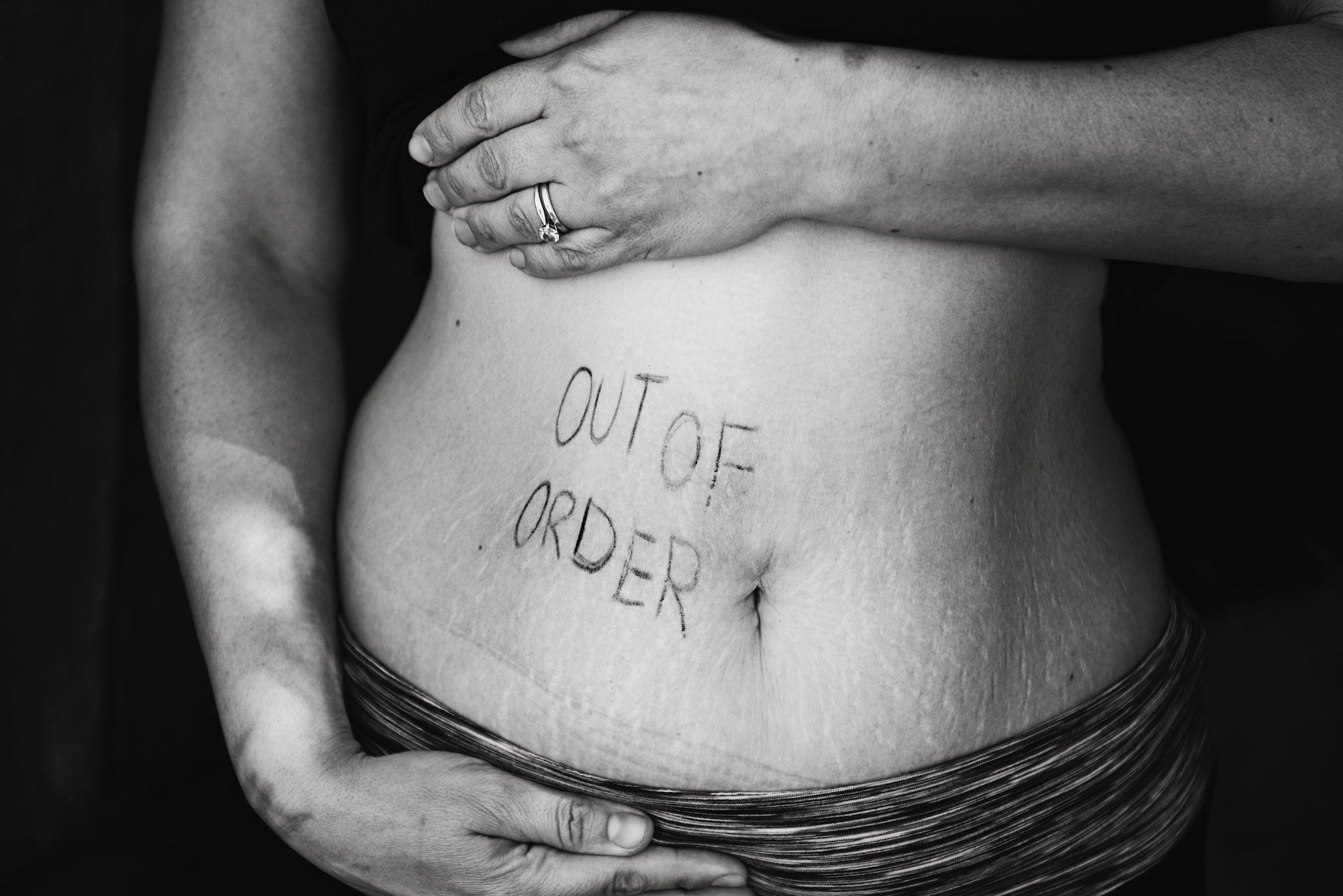
Crohn’s disease is characterized by inflammation that occurs in segments anywhere in the digestive tract, from the mouth to the anus.
What is Crohn's disease?
Crohn’s disease is characterized by inflammation that occurs in segments anywhere in the digestive tract, from the mouth to the anus. The most commonly affected area is where the small transitions to the large intestine. The inflammation caused by Crohn’s disease can cause damage to intestinal tissue that can lead to ulcers, strictures, fistulas, or abscesses. Moreover, if the colon is affected, patients at an increased risk of developing colon cancer.
What are the symptoms of Crohn’s disease?
- Cramps in the lower abdomen
- Chronic diarrhea, sometimes bloody
- Weight loss
- Fever
- Nausea
- Vomiting
- Gas
- Fatigue
If symptoms progress without medical attention, they can lead to more serious complications, like a bowel obstruction or lack of nutrients.
What causes Crohn’s disease?
While scientists have not yet discovered exactly what causes Crohn's disease, there is some evidence it could be genetic. A person is about 10 times more likely to develop the disease if a close relative has it.
How can Crohn's disease be treated?
Soluble fiber.
Dietary fiber can greatly reduce the risk of developing a Crohn’s flare up. The best option for those struggling with the disease is soluble fiber, which absorbs water as it moves through your gut, slowing digestion and reducing the risk of diarrhea. Insoluble fiber, on the other hand, can move through your system too quickly and with too much water, leading to diarrhea and cramps in some Crohn’s patients. (Keep in mind: Neither fiber is recommended to be eaten during a flare-up—just soluble fiber to keep flare-ups away.)
While you can get fiber from plant-based foods, it’s hard for most Americans to get enough: 95 percent of Americans don’t come close to the FDA recommended daily intake for fiber that can help manage Crohn’s disease. Supplements are an easy way to increase your fiber intake. Those with bowel issues like Crohn’s might consider Bellway, an organic soluble fiber supplement that doesn’t contain artificial ingredients, like many other brands do. (As you would with any supplement, check with your doctor that it’s right for you.)
Drug therapy.
In cases of Crohn’s disease, doctors typically prescribe drugs that will address the inflammation. For example, during an acute flare, cortisone or special anti-inflammatory may be administered. If frequent relapses occur, patients may be put on long-term medications.
Supplemental vitamins and nutrients.
People with Crohn’s disease may experience difficulties absorbing and retaining important vitamins and nutrients from their food, which then have to be supplemented through their diets. The most common of these lacking vitamins and nutrients include potassium, calcium, iron, magnesium, vitamin B12, folic acid, and vitamin D.

